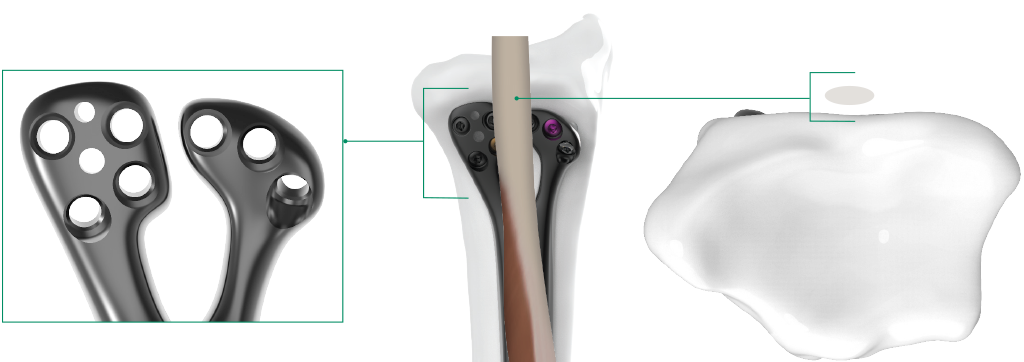
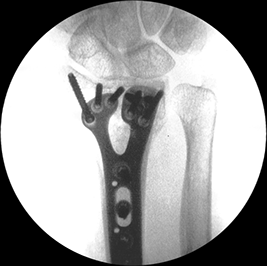
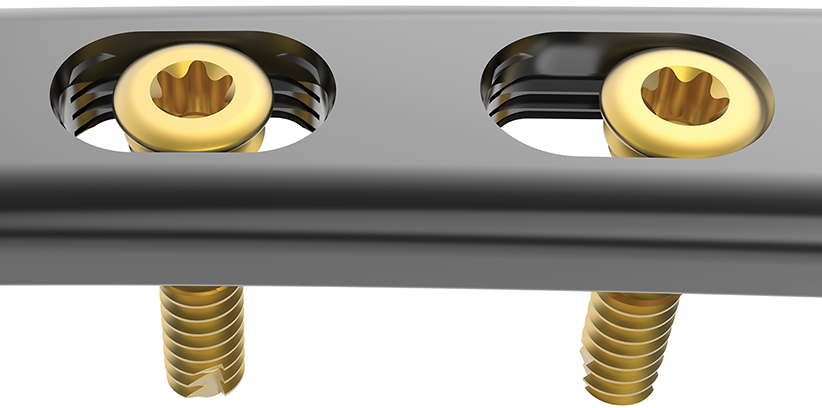
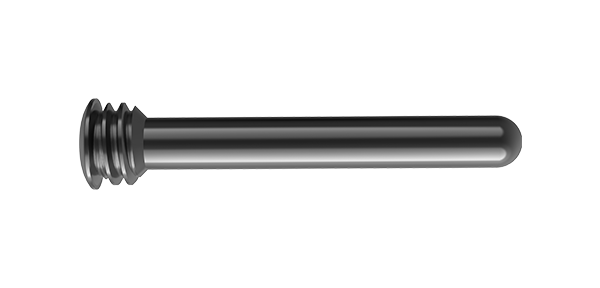
Dual head design protects flexor tendons by providing the lowest profile at the watershed line1
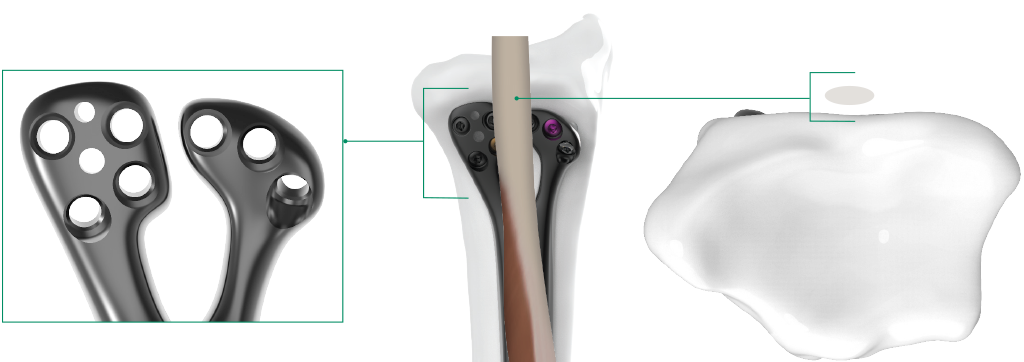
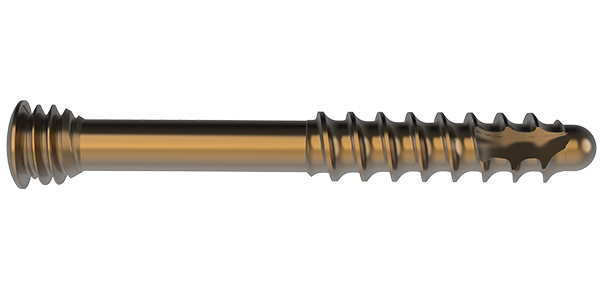
Screw trajectories designed to provide optimal subchondral support
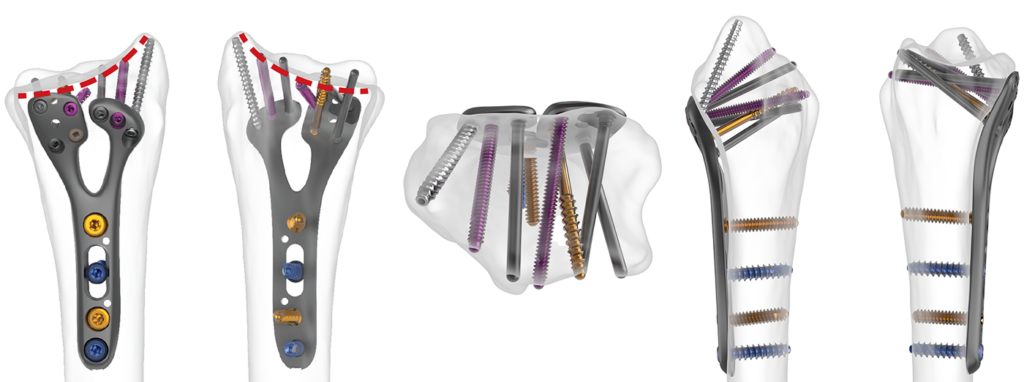
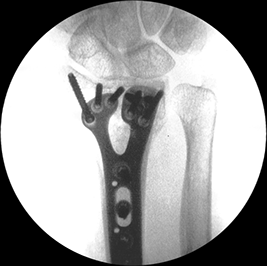


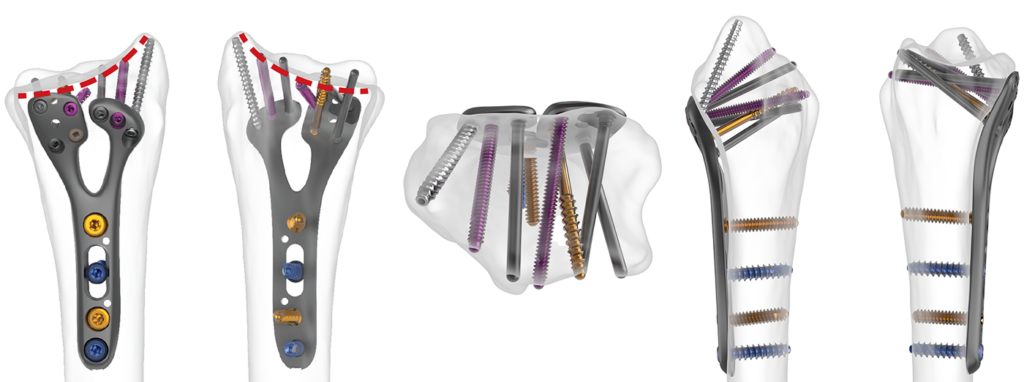





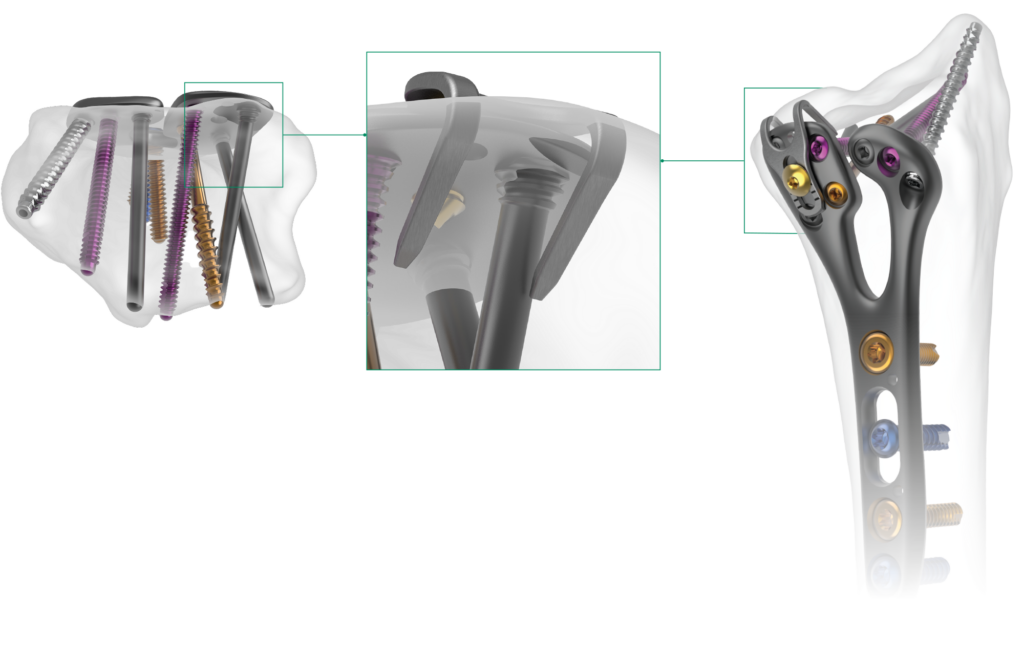

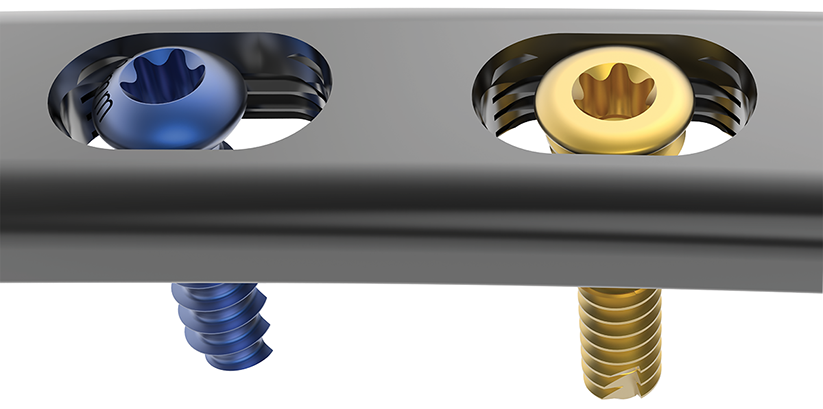
Both compression and locking screws can be inserted in any position in FreeFix® slots
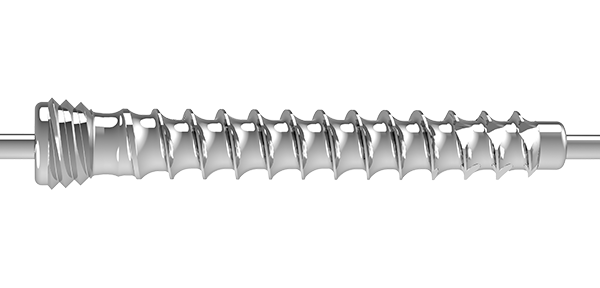
Patented horizontal thread pattern allows dynamic compression with locking screws
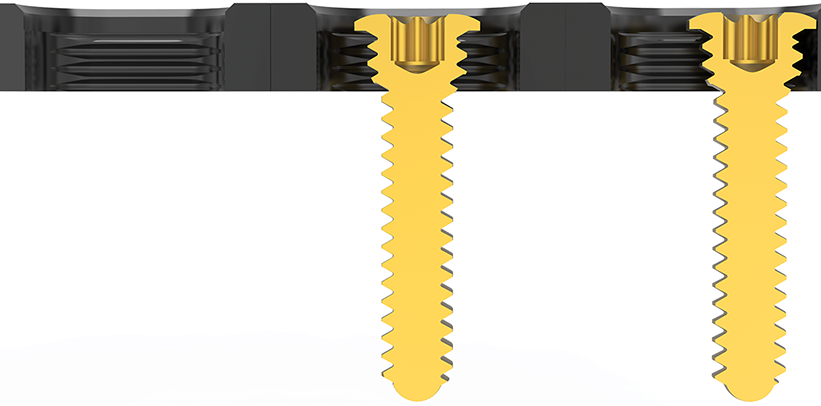
1.5mm of dynamic compression per slot










(Drag to rotate)
PUBLISHED CLINICAL DATA: 1Limthongthang R, Bachoura A, Jacoby SM, Osterman AL. (2014) Distal Radius Volar Locking Plate Design and Associated Vulnerability of the Flexor Pollicis Longus. J Hand Surg Am, 30(5): 852-860. DOI: 10.1016/j.jhsa.2014.01.038
2Salas C, Brantley JA, Clark J, Reda Taha M, Myers OB, Mercer D. (2018) Damage in a Distal Radius Fracture Model Treated With Locked Volar Plating After Simulated Postoperative Loading. J Hand Surg Am, 43(7): 679.e1-679.e6. DOI: 10.1016/j.jhsa.2017.12.019
3Orbay JL, Rubio F, Vernon LL. (2016) Prevent Collapse and Salvage Failures of the Volar Rim of the Distal Radius. J Wrist Surg, 5(1): 17-21. DOI: 10.1055/s-0035-1570745
4Orbay JL, Gray R, Vernon LL, Sandilands SM, Martin AR, Vignolo SM. (2016) The EFR Approach and the Radial Septum- Understanding the Anatomy and Improving Volar Exposure for Distal Radius Fractures: Imagine What You Could Do With an Extra Inch. Tech Hand Up Extrem Surg, 20(4): 155-160. DOI: 10.1097/BTH.0000000000000139
5Orbay JL, Badia A, Indriago IR, Infante A, Gonzalez E, Fernandez DL. (2001) The Extended Flexor Carpi Radialis Approach: A New Perspective for the Distal Radius Fracture. Tech Hand Up Extrem Surg, 5(4): 204-211. DOI: 10.1097/00130911-200112000-00004
6Orbay J, Shah A, White BD, Patel A, Vernon L. (2016) Volar Plating as a Treatment for Distal Radius Fractures. Plast Reconstr Surg Glob Open, 4(9): e1041. DOI: 10.1097/GOX.0000000000001041